Fighting COVID-19 in the Middle East, North Africa and the Philippines
The international aid organisations are currently engaged in corona responses all over the world, doing critical work and helping national governments, health authorities and patients overcome the pandemic. Their employees are doing lifesaving work, some as frontline workers and some in offices across the planet. We have asked two graduates from our master's programme in Disaster Management how they are dealing with the corona pandemic in their daily work and what the situation looks like in the Middle East, North Africa and the Philippines.

Fighting COVID-19 across the world from your home in New York
Brianna Katherine Martin is the International Rescue Committee’s Program Manager of the Middle East and North Africa, currently working from her home in New York. She completed the master’s programme in Disaster Management in 2015.
All of the countries in Brianna’s portfolio – Iraq, Jordan, Lebanon, Libya, and Syria – have been affected by COVID-19. Her organisation has mobilised a global corona response and Brianna’s job is to support and expedite processes for her brave colleagues who are risking their lives to fight COVID-19 on the frontlines. This means that she act as intercessor between country programs and donors, submitting requests to procure personal protective equipment and medical supplies, communicating on program suspensions and evacuations, and ‘decoding’ donor guidance on allowable emergency and program continuity costs. She further explains:
“We have also been working nonstop to help the country programs access new funds earmarked for pandemic response or redesign existing projects to include COVID-adaptive measures. These have included providing all staff with hygiene kits and prevention training, supporting health facilities to establish triage and screening spaces and procedures, and changing the way we conduct house visits, or distributions. Our Protection teams are also exploring remote and online case management and psychosocial support.”
Government restrictions threatens vital services
Governmental restrictions and curfews in the Middle East and North Africa are put in place to reduce the outbreak but it also means that other services – some lifesaving – by humanitarian programs and operations are being suspended. Brianna explains:
“In Iraq, for example, a national lockdown has been in place since mid-March, and movement between and within governorates is severely limited. Our Protection and Rule of Law programming includes legal guidance and representation for those wrongfully detailed. With the courts closed, the team is unable to open new cases or follow up on old cases. In northeast Syria, bank closures combined with border restrictions, is impacting hawala (informal value transfer system based on the network of money brokers) liquidity – and it’s proving impossible for NGOs to continue cash transfer programming, pay vendors and staff without functional hawalas. And across the region, school closures mean we’ve lost a valuable entry point for our Child Protection programming.”

Hard to control COVID-19 in informational settlements
Across contexts, informal settlements - including camps for the displaced and urban slums - will face significant challenges in controlling COVID-19. Transmission reducing measures like cutting back on physical contact and improving hygiene are simply less feasible in locations where dwellings are cramped, land ownership is extremely rare and the risk of eviction is ever-present. And when most of the population relies on daily participation in the informal economy to survive, governments can't simply issue a "shelter-in-place" order without accompanying economic assistance, Brianna explains.
“At the same time, informal settlements can be very organised, with their own governance and community support structures. COVID-19 response is going to vary by country, but one commonality I think we're seeing come out quite strongly, is that in these informal settlement contexts, successful mitigation and care efforts are going to have to build on these existing community structures.”

Lack of resources could overwhelm healthcare systems quickly
Capacity and resources differ across the Middle East and North Africa region, but overall the national healthcare systems do not have the resources necessary to fight the outbreak. We are seeing COVID-19 overwhelm healthcare systems in stable, developed countries, so the prospect of outbreaks in fragile and conflict-affected states should really drive us to act. Brianna further explains:
“Two statistics from recent International Rescue Committee publications come to mind here: the first is that there are 11 ventilators and 28 ICU beds across all of northeast Syria. Nearly all of the 30 ventilators in northwest Syria are already in use – and of course, hospital facilities and healthcare workers have been under siege, and deliberately targeted in air strikes there, for years. The second is a comparison of population density: on the Diamond Princess cruise ship, there were 24 people per 1,000 m2 on board, and the virus spread four times faster on the ship than it did in Wuhan. In Cox’s Bazar camp in Bangladesh, there are 40 people per 1,000 m2; in Moira camp, in Greece, there are 204 people per 1,000 m2. If we think about the similarly dense camps in the Middle East and North Africa – Al Hol in northeast Syria, for example – and densely populated urban centres filled with already-vulnerable refugees, this statistic is really alarming.”
The countries the International Rescue Committee is active in were dependent on external aid prior to this rapid onset crisis and this dependency has defiantly not decreased now. Resources are being mobilised for the COVID-19 response – through the United Nations’ Global Humanitarian Response Plan and bilaterally – but this funding needs to be directly channelled to NGOs already on the frontline, including local NGOs and Civil Society Organisations, according to Brianna. “I also feel really strongly that it’s the responsibility of big international NGOs to keep supporting our local implementing partners throughout the crisis, in areas like staff safety, resource needs and risk analysis and so forth.”
A potential “double emergency” in the Middle East and North Africa
Because of the healthcare system weakness, the population density, inaccessibility due to conflict, organisations are bracing for the worst in the Middle East and North Africa. “We’ve referred to it as a “double emergency” because of the immediate devastation an outbreak would have coupled with the long-term economic, social, and psychosocial impact on already vulnerable populations” Brianna explains.
“With movement restrictions, beneficiaries are struggling to access basic services. Prices of essential commodities may increase. Low-income earners, especially camp-based internally displaced persons and refugees, who often survive on casual labour, will face serious hardship. And in a lot of the countries in this region, there’s concern that non-state actors will exploit the political vacuum and panic caused by the pandemic” Brianna warms.
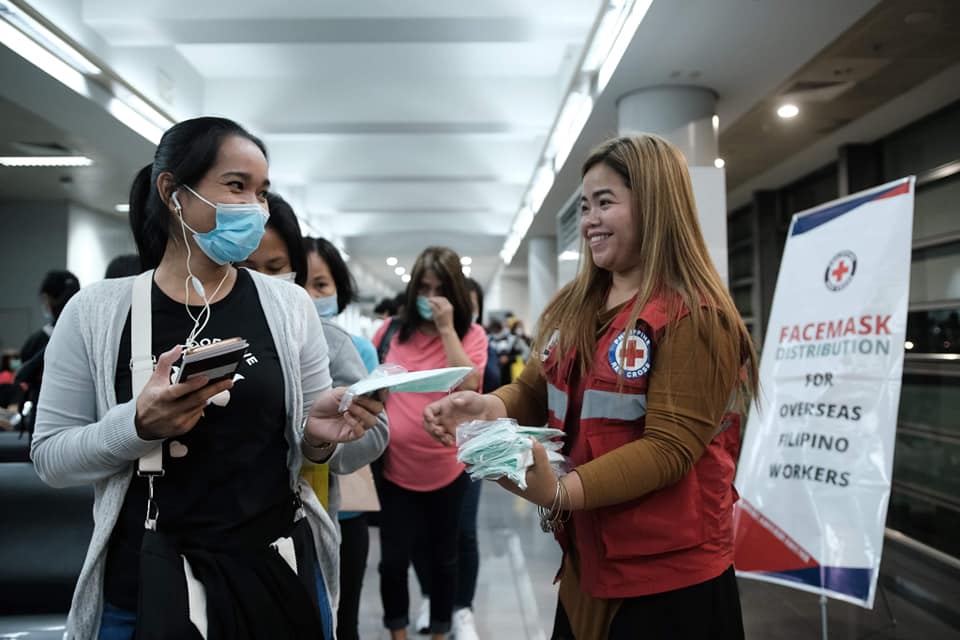
The COVID-19 response in the Philippines
Shir Shah Ayobi is the Red Cross’s Country Director in the Philippines. He completed the master's programme in Disaster Management in 2016. He reports on the current situation:
“The Philippine Government has implemented enhanced community quarantine for Luzon Island - the largest island that includes the National Capital Region severely hit by COVID 19 - effective from 15 March until 30 April. Effectively, this is a total lockdown and it means that the region is closed off from land, air, and sea travel. In addition, classes at all levels, mass gatherings and public transportation has been suspended. Government provided transportation to health workers and other frontline personnel as well as other private vehicles must apply for permission to operate. Social distancing are to be strictly observed and therefore, the Department of Labor and Employment encourages employers in the private sector to implement flexible work arrangements. Only food stores and pharmacies are open to serve the public.”
Preparing the healthcare system in the Philippines
“At the start of the pandemic, the Philippines’ hospitals were not geared and ready for this but within a few weeks, they made adjustments, additional supplies arrived from abroad and testing facilities have been increased” Shir Shah explains.
The human resources – doctors, nurses and other medical staff – needed to fight the battle against the virus in the Philippines are currently available and sufficient, according to Shir Shah, and facilities are improving their services and additional support from humanitarian and private sectors, individuals and other NGOs help the government in the fight.
It worth to mention that, the Philippine Red Cross is a major player in ramping up testing capacity using RT PCR (Reverse transcription polymerase chain reaction) machines to make sure that in the post lock down scenario, local governments can immediately test, identify contacts and isolate patients with infection. Philippine Red Cross has temporarily taken over the task of the national testing center from the Research Institute for Tropical Medicine, which had to shut down due to infections among the staff.

Philippine Red Cross is leading the way in pre-hospital care by heavily investing in COVID-ready ambulances with capacity for negative pressure and other forms of infection containment.
Shir Shah predicts that the number of COVID-19 patients will continue to increase at least until the end of June 2020. Although good hygiene practice exists in the Philippines, he is still worried:
“If social distancing is not followed, people can still easily get infected when they go to for example food markets and hospitals. Therefore it is important with continued hygiene awareness and discipline among people” Shir Shah explains. “Furthermore, it is important that people have access to media outlets and other reliable communication channels so they can stay updated on the situation”.
International support for the response in the Philippines
The country has a relatively stable economy and acceptable healthcare infrastructure but the country depends on external medical supplies and equipment. Funding for health facilities and humanitarian organisations, donation of supplies – personal protective equipment, testing kits and ventilators – to the health facilities as well as and food packages, cash, and hygiene kits to the communities is needed.
The Red Cross is working closely with the government and the health authorities in various ways. They have established of a 24/7 hotline, receiving calls from patients and worried citizens; they are mobilising volunteers to provide COVID-19 patients with adequate help; they are providing emergency medical tents at the health facilities as well as personal protective equipment and hygiene kits; they help with the installation of COVID 19 testing facilities; and provide ambulance services.
Furthermore, with their Community Action Plan, the Red Cross are providing cash and in-kind assistance to the most vulnerable households in the Philippines, which includes distribution of hot meals, psycho social supports, hygiene promotion activities and installation of hand washing facilities.

Read more about our master's programme in Disaster Management here.
Topics
News

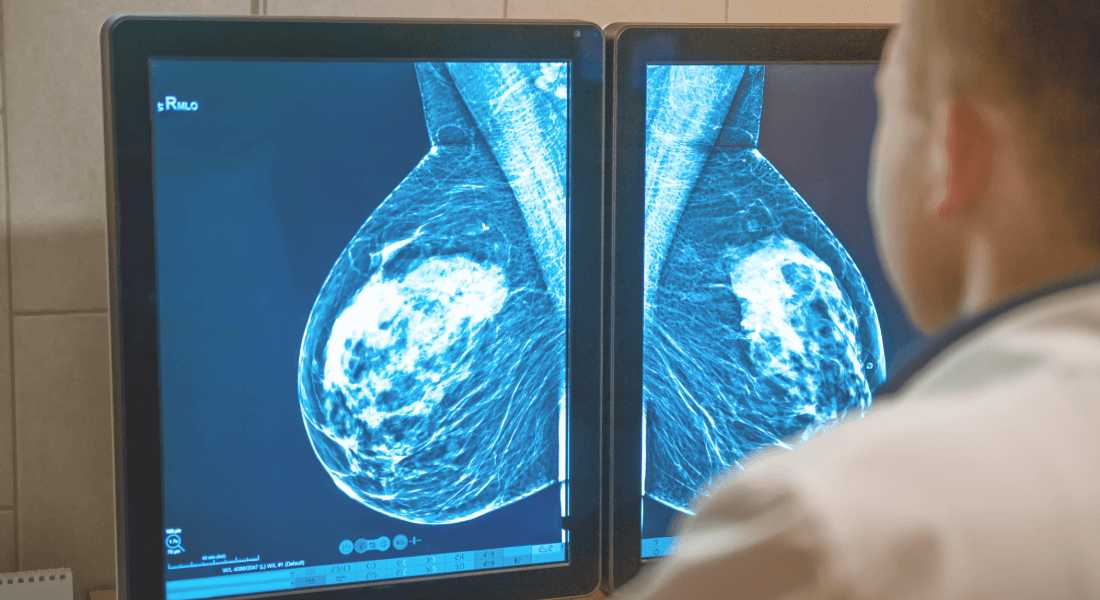
More women can now get answers about their hereditary risk of breast and ovarian cancer due to new genetic method

Understanding cancer cell subclones opens door to more personalized treatment